Declare rejected citing dwelling isolation
The case pertains to the rejection of a medical declare on the bottom that the affected person was asymptomatic and will have been handled at dwelling. The grievance was filed by Dadri resident Nitu Nagar on September 1, 2022, earlier than the district shopper disputes redressal fee (DCDRC).
Nagar mentioned her husband, Ajay Nagar, had been coated below Star Well being’s Household Well being Optima Insurance coverage Coverage since 2018. The coverage had been renewed yearly with no break.
Hospitalisation throughout fourth yr of coverage
The declare was raised in January 2022 in the course of the fourth yr of the coverage. Nagar was admitted to Yatharth Hospital in Better Noida after she developed excessive fever and respiration problem. The household felt rapid hospital care was wanted.
As per coverage guidelines, the insurance coverage firm was knowledgeable earlier than admission. The household was advised that the cashless declare could be accepted in a number of days.
Declare denied after hospital discharge
Later, the insurer refused to clear the hospital payments. The entire expense got here to Rs 49,423. The household paid the quantity from their very own pocket and utilized for reimbursement. When the declare was not settled, Nagar despatched a authorized discover to the insurer on August 3, 2022. There was no response.
Insurer cites coverage circumstances
Throughout the listening to, Star Well being submitted that it acted as per the coverage phrases. The corporate mentioned that the cashless request was reviewed however the medical paperwork confirmed solely easy complaints resembling fever and physique ache.The insurer mentioned the affected person had asymptomatic Covid and didn’t require hospital admission. It added that as per authorities tips, such instances may very well be managed at dwelling. On this foundation, the corporate defended its choice to reject the declare.
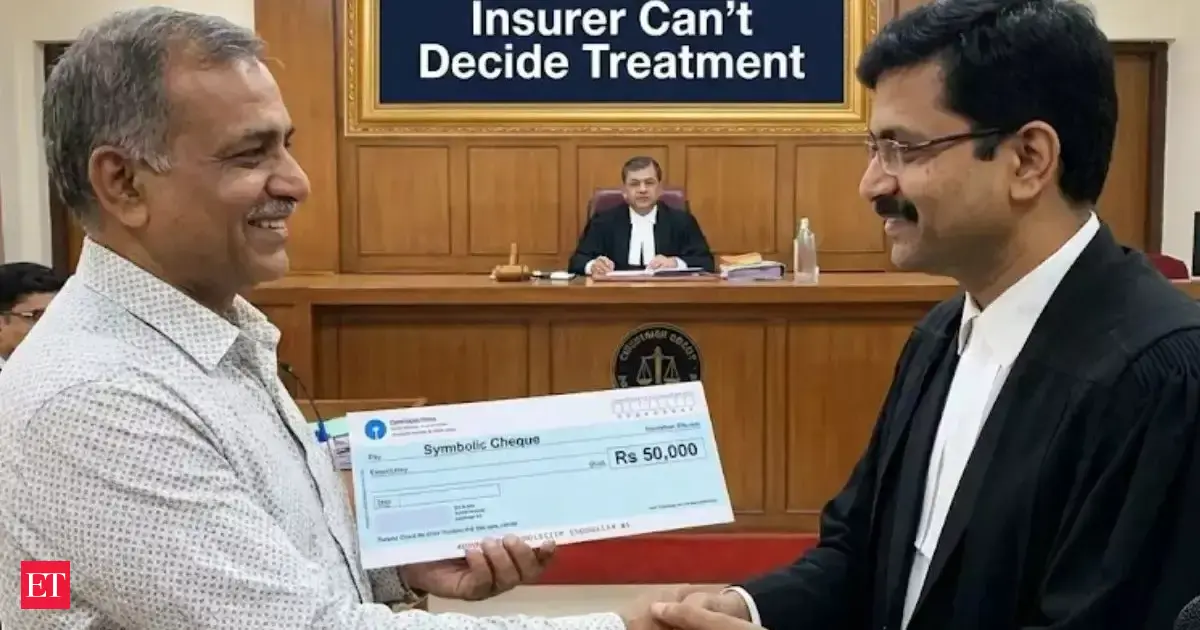
Fee rejects insurer’s stand
In its order dated November 26, fee president Anil Kumar Pundir and member Anju Sharma dominated that an insurance coverage firm can not override a physician’s choice.
“If medical specialists deem hospitalisation vital, they mentioned, the insurer can not insist that remedy be carried out at dwelling.”
The fee additional mentioned, “Rejection of the declare on the bottom that the affected person ought to have obtained remedy in dwelling isolation is a deficiency in service on the a part of the insurance coverage firm.”
It directed Star Well being to reimburse the hospital costs together with curiosity and litigation value.